Jennifer Hunt and Mike Dunaway stand beside a patient lying in a hospital bed.
“You can feel right here … press real gently and you can feel his pulse,” Hunt said. “You see his chest is rising and falling as he’s breathing.”
“His eyes will dilate,” said Dunaway.
“He blinks at you,” Hunt added.
A monitor tracks this patient’s heart rate, heart sounds, oxygen saturation, blood pressure, respiratory rate, and how fast he’s blinking. He coughs. He sweats. He cries. He urinates. He vomits. His lips turn blue if he doesn’t get enough oxygen. He can be intubated, catheterized, given medicine, and hooked up to an IV.
He speaks to tell you when something hurts.
The pair are not observing a live, human patient, and they are not in a hospital. Hunt and Dunaway are standing in a first-floor simulation lab at the Murphy Deming College of Health Sciences and are demonstrating the school’s high-tech patient simulator, the “Cadillac of mannequins,” or SimMan 3G, to be more precise.
Now in their third semester at Murphy Deming, students in the Master of Science in Physician Assistant (PA) program are ramping up their hours inside the lab working with human-like simulators like this one to enhance their classroom and clinical experiences.
The simulation center gives students an opportunity to practice clinical skills without using real patients. Students identify and implement medical procedures on the mannequins without risk and can reap the “benefit of learning from failing,” says Hunt, assistant professor of PA.
“The Sim Lab is modeled after a hospital environment,” said Dunaway, interprofessional simulation center coordinator. “Obviously they are not real patients. That’s the advantage of having the mannequin is that you can program the unit and present a lifelike scenario for patients to react to without worrying about a human subject being involved.”
Hunt jumped in: “Those ‘do-not-miss, it-will-kill-the patient-if-you-miss’ kind of scenarios are an important part of the clinical education experience.”
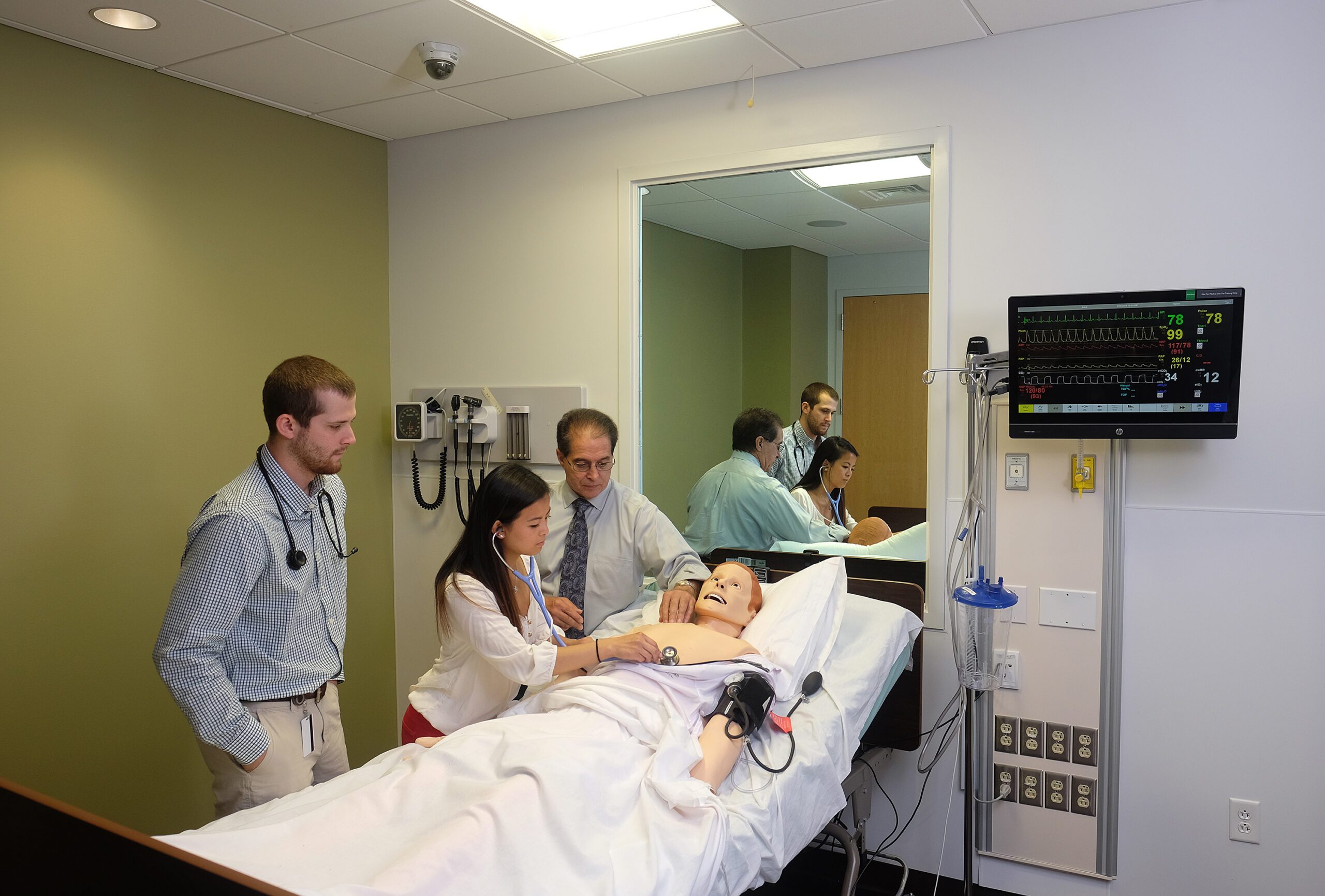
While students provide clinical care to SimMan, an instructor is in an adjacent control room running the simulation scenario, which responds to the actions of the student caregiver. It’s ideal for testing purposes. Everything is recorded so that when students are debriefed after the simulation — either by the instructors or by their peers — they can see exactly what happened.
“We can control what the blood pressure is, what the heart rate is,” Hunt said. “Are they doing it properly? Can they identify the abnormal?”
PA students are developing higher skills, moving from simply identifying the abnormalities, to running more advanced lessons on the mannequin. The experiences in the Sim Lab are often combined with live patient observations in the clinical setting or simple clinical exams and procedures in the exam rooms at Murphy Deming.
In both settings, students are also learning soft skills — for instance, how to talk with a patient — along with clinical skills, such as starting an IV.
In addition to SimMan, there is also SimMom, another high-fidelity mannequin with a uterus and fully articulated limbs, can simulate a woman in childbirth. Students can practice both standard as well as cesarean deliveries and instructors can run more complicated scenarios — obstetric emergencies like a breech presentation or retained placenta — to keep students on their toes.
“Not every student is going to get to see a baby delivered when they’re out doing their OB-GYN rotation … so they have the opportunity at least to experience it in this setting so it can supplement and make up for some of the gaps they might have in their clinical year,” Hunt said.
In a third exam room, there is SimBaby for pediatric training.
“And this is Peanut,” Hunt said, gesturing to the life-like infant simulator. The mannequin has soft spots on top of its head that can retract or bulge based on blood pressure. SimBaby can be monitored with a tiny blood pressure cuff and oximeter and can be given an intraosseous port for delivery of medicine.
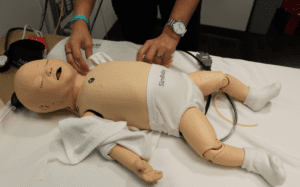
Again, the simulation lab provides PA students additional opportunities to work with babies and women.
In addition to working on the full-size mannequins, students also have the benefit of learning more specific set of skills on “task trainers,” which can be as simple as a sound pad for monitoring heart sounds to complex trainers for IV placement and chest tubes.
Lower-tech full-size simulators that have more mobility are more frequently used by students in Murphy Deming’s occupational therapy and physical therapy programs.
In addition to the simulated hospital rooms at Murphy Deming, there are exam rooms that are set up like those in a doctor’s office. Students will often practice a specific function on the task trainers inside those rooms. Other times, they will use the spaces to perform exams on real-life patient volunteers under the supervision of a PA or a doctor.
The lifelike hospital rooms; high-tech patient simulators; top-notch faculty; and an innovative, interprofessional teaching model provides Murphy Deming students with an essential learning tool that will support them in becoming outstanding clinicians.